Over 1 billion people live in poverty and have less than $2 per day at their disposal. These people (one in six of the world’s population) usually live in rural areas and are inevitably mired in poverty because of poor health, especially chronic diseases caused by infection with parasitic diseases now known as ‘Neglected Tropical Diseases’ or NTDs.
In 1985 a drug donation of mectizan (ivermectin) led to a mass drug administration to over 100 million people a year in Africa to protect them against river blindness. Where once 50% of people over 40 years of age were blind today they all have their sight. By 2013 several more donation commitments have been made by several pharmaceutical companies with the result that the 1 billion poor people in need of drugs can now receive them free of charge.
Through mass drug administration for NTDs, the Schistosomiasis Control Initiative (SCI) at Imperial College has played a leading role in reaching out to the poorest people in Africa and improving their quality of life. While many have been reached already, more support is needed. Thanks to the pharmaceutical industry the necessary drugs are available, but the challenge now is to deliver these drugs to recipients at the end of the road in developing countries.

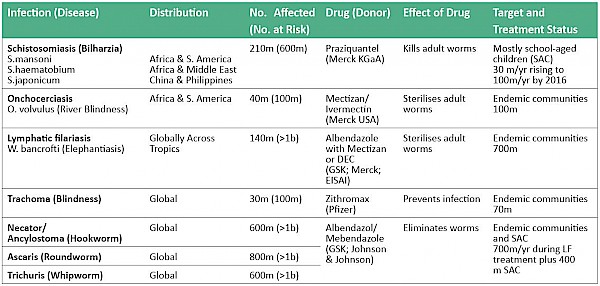
There are seven Neglected Tropical Diseases which are targeted for elimination by 2020 by the member states of the World Health Organisation – and all seven can be treated with safe oral drugs usually distributed annually. However the treatments do differ from disease to disease and country to country based on epidemiological data, disease distribution and in some cases intensity of infection. The World Health Organisation has promoted the concept of ‘Preventive Chemotherapy’ (PCT) by which the drugs below, donated by the pharmaceutical industry, are distributed annually throughout the endemic areas in order to improve the health of those infected, reduce transmission and head towards elimination of these dis- eases by 2020. The WHO has made such information available to relevant Ministries of Health and supported all the efforts of the Schistosomiasis Control Initiative (SCI) at Imperial College to improve coverage against NTDs.
The SCI was established in 2002 with a grant from the Bill and Melinda Gates Foundation which was used to implement programmes in six countries: Burkina Faso, Mali, Niger, Tanzania, Uganda, and Zambia. In 2006 the SCI expanded to cover Burundi and Rwanda. In 2010 funding from the UK Aid Agency DFID allowed SCI to expand in to Cote D’Ivoire, Liberia, Malawi, and Mozambique. Additional private funding allowed SCI to assist Madagascar, Mauritania, Senegal, and Zimbabwe. Finally the World Bank called on SCI for assistance for its programme in Yemen.
SCI has been one of the strongest advocates for PCT and has assisted in raising global awareness of these diseases, raising funds for delivery of the drugs in each of 16 endemic countries, and offering technical assistance to ensure country-wide mapping to improve optimum use of the drugs, training of health personnel, teachers and community volunteers. This ensures that the necessary drugs reach the poorest people in remote areas with the greatest need. However, the mechanism for getting the donated drugs from the factory gate to the mouths of those in need is complex and requires sophisticated planning and logistical support.
Rapid Expansion of Treatment
As recently as 2000 there were no treatments against schistosomiasis or intestinal helminths in sub Saharan Africa, and trachoma and LF treatments were just starting. In contrast, by 2013 over 700 million treatments had been delivered. These programmes have expanded so much that in 2013, the World Health Assembly passed a resolution calling on all member states to move towards the elimination of Neglected Tropical Diseases by 2020. As shown above, the drugs which are needed to treat all the target populations are available on request, and so the challenge is how to reach rural communities in which the prevalence of these diseases is at the highest level.
Prior to 2006, the main donor for NTDs was the Bill and Melinda Gates Foundation – un-doubtedly they opened the door for initial drug distributions to reach some remote rural populations infected with these diseases. Since 2006 there have been two major donors, plus a steady stream of smaller donations, to fund the delivery of these drugs from the port to the recipients. Major do- nations have come from the United States Agency for International Development (US- AID), and from the Department for International Development (DFID) in the UK. Other donors include the World Bank, the ENDFUND (based in the philanthropic organisation Geneva Global) and from the general public in both the USA and UK, and to a lesser degree from other developed countries.
If we examine these large donations: USAID have awarded $250 million over 5 years to the Research Triangle International (RTI), who in turn use several implementers on the ground to assist Ministries of Health (MoH) to deliver the donated drugs. USAID have awarded a further $200 million to Family Health International (FHI), who in turn use implementers to assist MoHs to deliver donated drugs. RTI work in some countries and FHI are allocated other countries. The World Bank has a number of supporting initiatives helping both the Ministries of Health and Education with health system strengthening. For example, the World Bank are providing all the funding necessary to purchase and deliver drugs targeting schistosomiasis in Yemen. The budget for this one country is $25 million over 6 years, and the SCI is providing the technical assistance needed.
$2 billion might be all that is needed over the next seven years to fund the distribution of donated drugs throughout sub Saharan Africa
In addition, the SCI has been fortunate to be recognised as a “value for money” charity by UK and US charity evaluators, www.givingwhatwecan.org and www.givewell.org. Their recommendations to the public, who wish to give to a cost effective charity, have led to over £2 million in donations to SCI to help start up programmes in several countries.
Looking towards the goal of elimination by 2020, it has been estimated that perhaps $2 billion might be all that is needed over the next seven years to fund the distribution of donated drugs throughout sub Saharan Africa. Of this, about half has been pledged by the above organisations.
Manufacturer to Mouth
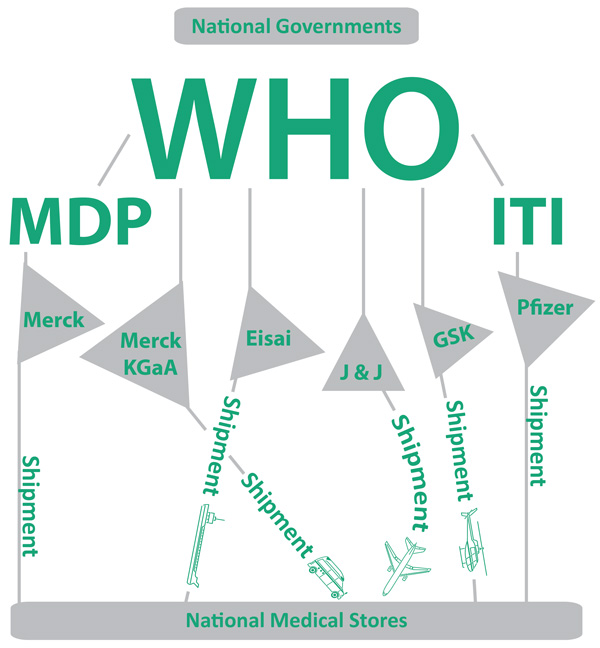
Prior to 2010, each of the drugs had to be applied for separately according to need in each individual country. Since 2010, there has been a mechanism developed to simplify the application process as shown in the schematic above. Pfizer and Merck USA have their own separate processes for approval of donations – Pfizer operate through the ‘International Trachoma Initiative’ while Merck USA use the ‘Mectizan Donation Programme’ both based in Atlanta within the Task Force for Global Health.
However, all requests must come from individual country governments (not from NGO’s) through the World Health Organisation who use a regional review panel to evaluate all requests before passing the orders on to the respective manufacturing companies.
Drugs are often imported to the recipient country with the assistance of the World Health Organisation country representative, and then delivered to the respective National Medical stores. From the stores, nationwide drug distribution is the responsibility of the Ministry of Health.
With funding from major donors, as explored in the previous section, MoHs implement drug distribution programmes with the help of Non Governmental Organisations (NGOs) which are responsible for accountability, for providing technical assistance, and for monitoring and evaluation after treatments.
So what does a Neglected Tropical Disease (NTD) implementation programme look like? There are several critical path steps for a country to implement an NTD programme aiming for elimination by 2020, and these are:
Mapping
- To determine the distribution of the various NTDs in the country – these diseases are not evenly distributed and we need to know where the diseases are to be found and indeed where they are not, so that we can plan treatments by district.
Stakeholders meetings
- To determine what resources are needed, what are available and what the resource gaps are. To agree a strategy for treatments by district – and from there determine the drug needs. Agree distribution of work and responsibility be- tween stakeholders. Order drugs for each NTD
- Determining how many drugs to order is no easy matter, and of course the lead time to delivery is at least 6 months.
Training
- A timetable and curriculum for all the training needs is required. Training should be directed to all levels – central scientists responsible for the programmes through to regional directors, health personnel, teachers and community drug deliverers.
Logistics
- Arrangements for transport of not only the drugs but also all the other equipment that is required such as microscopes, haemacue machines, dose- poles etc.
Advocacy (sensitization)
- Every official likely to be involved in the drug distribution needs to be fully informed to ‘keep them on board’. The people who will actually dispense the drugs need training and to know where and when to collect their drugs. The target population need to be given information about the campaign and the benefits of taking the medicines offered. MDA (Mass drug administration)
- The drugs are administered according to the agreed protocol to either school children through the schools, to school-aged children, which means a strategy is needed for reaching children outside school, and the whole community where appropriate. Provision must be Monitoring and Evaluation
After treatment - a coverage survey is required to confirm effective drug delivery. Monitoring of any unwanted side effects. 6 month or 12 month follow up to monitor drug efficacy. Thus, it is clear that very large drug donations is just one part of an elimination strategy - it is necessary to have in place mechanisms for reaching out to recipients and ensuring good coverage (over 75%) if the programme is to be successful.
Towards Elimination
With these fantastic drug donations, parasitic diseases such as schistosomiasis are en route to elimination in terms of both morbidity and transmission. Co-ordination between the Gates Foundation, WHO, USAID, The World Bank and DFID and implementers such as SCI ensures that available resources are used carefully and efficiently, and duplication of effort is avoided.
Currently the main push is to expand in the large countries of Africa such as DRC, Ethiopia, Nigeria, Tanzania and Mozambique, and when national coverage is achieved in all of them we will be well on the way to elimination. However the last mile will be reached only when water supplies are improved, sanitation is much more widespread and latrines are used.
However, by 2020 we can expect to be much nearer our goal thanks to the pharmaceutical industry, the funding agencies and implementers – but most of all because of the increased awareness and political commitment of the developing countries to eliminate these diseases.









