If you have ever a received a text-message reminder for a health appointment, then you have already experienced mobile or mHealth in action – but this is only the beginning. In the future, smartphones, apps and connected sensors will increasingly be used to support all aspects of health. As these technologies become prevalent there is a need to make sure they are effective and safe, but also to understand the implications for individuals and communities who will increasingly be asked to take charge of aspects of their own health.
In 2007, a new era of personalised computing dawned with the launch of the smartphone. Capitalising on advances in displays, sensors, and miniaturised computing, this new generation of mobile phone introduced the app; a simple mechanism to add new functions on demand. Easily downloaded from online marketplaces, apps have proven extremely popular. The number of available apps can be measured in hundreds of thousands, and cumulative downloads in billions. Almost fifty percent of US adults now have a smartphone capable of running apps and the average user has installed over 40 apps on their device, spending around 40 minutes using them each day1.
Almost immediately, there was interest in how apps and smartphones could be used for health. Amongst researchers, it had been recognised for a number of years that emerging networked technologies would have uses for what would become termed ‘mobile’ or ‘m-Health’. However, it was only with the advent of smartphones and apps that mHealth began to gain wider attention amongst clinicians and policy-makers.
Driving this was, and is, a fortuitous intersection of three elements: novel technologies, a consumer phenomenon, and prevailing political priorities affecting health. While most people in developed economies will be smartphone owners by 2020, with developing settings not far behind, the phenomenon of the smartphone is more than one of scale: there has also been a shift in how people use such devices. For most, mobiles are now always-carried and always-on, raising the prospect of health-related services that integrate into the routine of daily life.
In developed settings, political priorities reflect the growing costs of healthcare and the increasing prevalence of long-term conditions associated with lifestyle and aging; for example, diabetes and dementia. As a result, policy-makers are actively searching for methods to reduce costs by reducing unscheduled or inappropriate use of services, increasing self-care, and focusing on preventative healthcare. The possibility that large numbers of patients could provide their own multifunction healthcare device would have seemed impossible even 10 years ago and yet now we have witnessed a UK health minister suggesting that smartphone apps be routinely offered “on prescription” for long-term conditions2, and the US Secretary of Health and Social Services declaring that “the greatest technology breakthrough of our time, will ensure that ‘control over your health is always within a hand’s reach’.3” Lifestyle-associated diseases are also increasingly relevant in developing settings, but mHealth efforts here are also concerned with infectious diseases like malaria and HIV, maternal and child health, and limitations in existing health infrastructure and workforce capacity.
The possibility that large numbers of patients could provide their own multifunction healthcare device would have seemed impossible even 10 years ago
Putting mHealth to work
Although some apps are designed solely for clinician use, for example as calculators to help work out drug prescriptions, the business of mHealth will take place somewhere in the space that exists between patients (and the public) and health care professionals. The range of potential applications is extremely broad.
Instead of booking a face-to-face consultation, a patient with a minor complaint might be able to seek advice from their clinician using a smartphone app. Problems might be resolved using secure text-based and email messaging, with the option of speaking by phone or using videoconferencing if further discussion is required. The device camera can be used to exchange images, while standardised questionnaires presented within the app could be used to assist the diagnostic process. An app might be able to offer video or audio guidance about what to do in an emergency, helping people provide appropriate first aid as well as decide where to seek help. In settings where access to primary care is limited, such services may be transformative. For example, a smartphone microphone can become a rapid diagnostic test for childhood pneumonia, a condition with high rates of mortality in remote settings4. mHealth can also help with the routine business of interacting with health services for example, booking appointments, ordering prescriptions and completing health checks, for example by offering text message reminders or app-based booking services that offer convenience and help reduce missed appointments.
mHealth has a role to play in self-care and medication management for long term conditions, for example asthma or heart failure. Taking advantage of the fact that smartphones are always carried, an app might act as a convenient diary for logging symptoms and measurements. Summarised graphically, the information that is collected can be used to help people make decisions about their own day-to-day treatment, perhaps stepping up an asthma inhaler in response to a dip in measured lung function. It can also help highlight changes that might need medical attention, for example, detecting the gradual gain in weight that signifies worsening heart failure. mHealth technologies can also offer access to education and information about a condition and, when required, additional peer and expert support through social networks. Text messages can be used to send bite-sized, tailored information, while apps can offer a full range of multimedia content. Many people with long-term conditions find it hard to take their medication reliably13. An app might be used to provide reminders about medication taking, and keep a log of medication- taking and side effects that can be used to start a discussion with a clinician. Text messages have been used successfully to remind people with HIV in Kenya to take their antiretroviral medication5.
Emerging sensor technologies will complement the functions offered by devices like smartphones. Indeed, the roots of mHealth lie in the world of novel sensors rather than the consumer technologies that have followed. The battery of sensors already in smartphones can already be used to measure heart rates (using the camera to detect changes in the light absorption of skin as blood is pumped through it with each heart beat6), detect falls, monitor activity levels, and diagnose changes in symptoms in conditions like Parkinson’s disease. But much more is possible. Sensors woven into clothing or integrated into wearable artefacts like watches, affixed to the skin, worn as a contact lens7, or even inserted subcutaneously, can track parameters like temperature, oxygen saturation levels and blood pressure and blood measurements like glucose. Combined with other information using a smartphone provided by the user, they can help people with diabetes or hypertension adjust their own medication or send automated alerts to health providers in an emergency. A tablet with a miniaturised, biocompatible wireless circuit could transmit a signal to let a smartphone track medication use, perhaps measuring and transmitting information about activity levels as well as drug metabolites in the gut8.
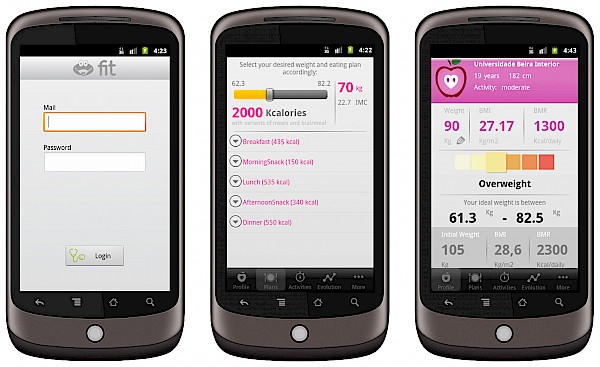
mHealth has also found applications in health promotion and behaviour change. Apps and text-messaging can be used to provide tailored support for people trying to stop smoking or lose weight. An app equipped with appropriate video or written messages can be used to provide motivational support to help people overcome cravings or low will-power ‘in the moment’. Rewards and visual feedback like exercise-completion badges or ‘money saved since quitting’ totalizers can be used to help people sustain behaviour by indicating progress towards a goal. Future apps might also be able to use local information to help people make healthy choices, for example by flagging a walking route to work as an alternative to driving as the user leaves the house (having automatically checked that the weather is suitable for walking).
Finally, there is an emerging role for mHealth in health surveillance. Internet-connected smartphones and tablets can speed up information collection from field workers, both as part of routine disease and public health surveillance, and in the aftermath of humanitarian disasters. Current work is also exploring the feasibility of ‘crowdsourcing’ such information, for example by sending text-messaging questionnaires to new mothers as part of child health surveillance in China9.
Challenges for mHealth
Despite its promise, mHealth faces substantial challenges. Perhaps the most pressing is the need for robust evidence that the range of applications can work in practice, at scale10. This means identifying how apps and other mHealth tools can fit into both clinical care and everyday life, and designing suitable evaluations – including randomised trials – that will take a whole systems approach to understanding their impacts, both positive and negative. Generating more data about individuals may usefully inform clinical decisions (and inform secondary ‘big data’ type analyses that can drive policy-type decisions) but it will also involve changed work practices for clinicians receiving those data, and unless tools are introduced to manage those new data flows, increased workload. Clinical models of disease management that are not predicated on such high-frequency, high-resolution data may be poorly adapted to distinguishing the signal of real problems amongst the inevitable noise that will result.
At an implementation level, there is much that remains uncertain, for example, about the best ways to target mHealth towards particular groups and address the rapid pace of technology turnover. One example of such turnover is the recent blurring of apps into services that you can access on multiple devices, through the web and on traditional desktop computers. For healthcare, with understandable sensitivities about privacy and security, this raises concerns about how to secure such information as it shared across the cloud whilst making sure it remains accessible to those who need it. Efforts to standardise protocols for exchanging information, as well as an emerging approach towards regulation, by both the US Food and Drug Administration and European regulators will play a role.
In some areas, regulation may be overdue. For example, diagnostic inaccuracies have been found in apps offering services to analyse images of possible skin cancers11. Safety risks are clearly present when apps are providing services like diagnosis or offering treatment decisions, but can also arise in unanticipated ways whenever systems change as a result of a new technology being introduced. A balance must be struck, however, between clinical risk and the potential to stifle innovation by creating costly hurdles through regulation and certification.
Putting the ‘me’ in mHealth
Although evidence gaps and safety impacts are important, identifying and addressing them forms part of the
routine landscape for most new health technologies. A
defining issue for mHealth
is the potential impact that
it will have on patients and
the public. It is us, as op
posed to clinicians, who will
have to ‘do’ mHealth as our devices, and time, are taken up for medical purposes, however unobtrusive and subtle the technology. Individuals and clinicians may hold a shared goal of better health, but there are different ways of achieving this that alter the balance of responsibilities expected of each. mHealth shifts that balance decisively towards the individual.
Text messages have been used successfully to remind people with HIV in Kenya to take their antiretroviral medication
There is no easy answer as to whether that is a good thing. In settings where healthcare provision is limited, the arrival of tools that help individuals manage their health might be welcomed. In settings with established provision, technologies that emphasise self-care and consequently reduce traditional forms of providing support, for example face-to-face consultation, might prove less acceptable. Some may find remote management convenient, whilst others see the loss of a source of social support offered by routine contact with a professional. Access to tailored education and tools may help individuals make ‘better’, more autonomous choices about their health. However those with limited health literacy, or literacy full stop, may not be able to realise those benefits. Certain monitoring data might be extremely useful to a clinician making dis- ease management decisions, but a patient might simply want to get on with the business of living their life without having to record information that serves as a reminder of their ill health. Part of the mHealth evidence gap concerns empirical data that captures the extent and distribution of such attitudes, although efforts are currently underway12.
At a provider and governmental level, there is understandable interest in technologies that might reduce healthcare utilisation and costs. In insurer-based systems it is easy to envisage the quid pro quo that might result: reduced premiums in return for a little mHealth-supported preventive healthcare. Such programmes may yet prove effective, but it is worth considering the extent to which individuals from poorer socioeconomic backgrounds really have a choice about whether to take up such offers. Discreet, pervasive monitoring might be seen as liberating by some, but raise unwelcome privacy and ethical implications for others. If the kind of consolidation that has characterised developments in internet search, social media and music affects health then there will be also be legitimate concerns about the hosting and processing of personal medical information by transnational corporations. Any data collected will have commercial and research uses for ‘big data’ population-level analyses, however the nature and extent of what is acceptable has yet to be explored.
mHealth offers an exciting breadth of possibilities for improving healthcare. The resulting technologies will undoubtedly benefit people, but they also create new demands that shift responsibilities for health away from clinicians. The debate about how best to balance those demands in ways that are both acceptable and equitable has only just begun.








